Knee pain can be a significant barrier to enjoying everyday activities, whether it's climbing stairs, running, or even sitting for long periods. One of the most common causes of knee discomfort is Patellofemoral Syndrome—also known as "runner’s knee." This condition affects people of all ages, particularly athletes or those who lead active lifestyles. Understanding its causes, symptoms, and treatment options is the first step toward finding relief.
In this blog, we’ll take a closer look at what Patellofemoral Syndrome is, how it develops, and the most effective treatment strategies to get you back on your feet.
What is Patellofemoral Syndrome?
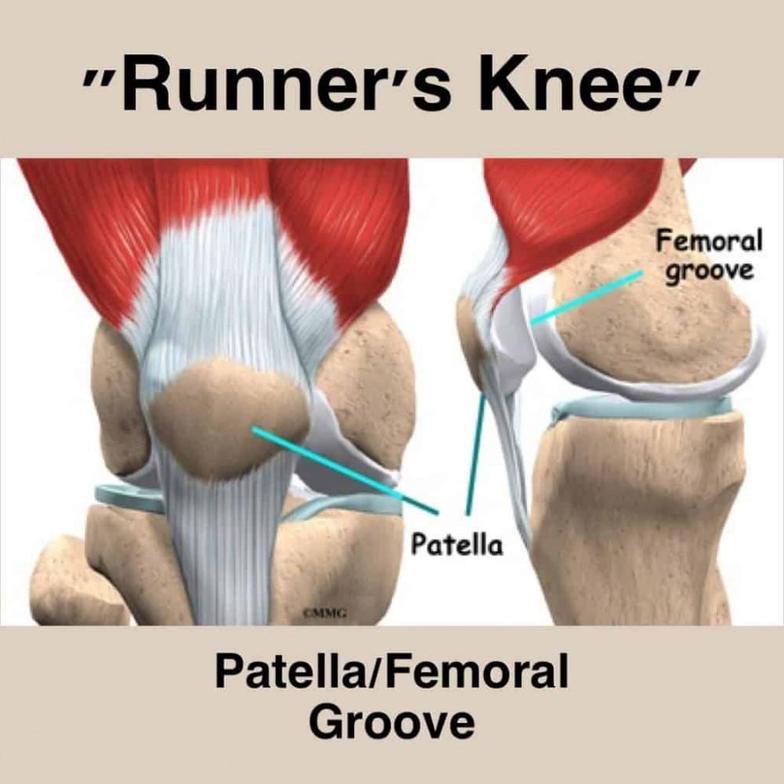
Patellofemoral Syndrome (PFS) refers to pain around the front of the knee, specifically where the patella (kneecap) meets the femur (thigh bone). The pain arises when the patella doesn't move or track properly in the femoral groove, leading to friction, irritation, and inflammation.
Causes of Patellofemoral Syndrome
Several factors can lead to the development of Patellofemoral Syndrome:
- Overuse: Repetitive activities like running, jumping, or squatting can place excessive stress on the knee joint, causing irritation.
- Muscle Imbalances: Weakness in the quadriceps, hamstrings, or hip muscles can lead to improper alignment of the kneecap, contributing to PFS.
- Injury or Trauma: A direct blow or injury to the kneecap can cause misalignment, resulting in pain.
- Structural Abnormalities: Flat feet, high arches, or other anatomical issues can increase the risk of developing Patellofemoral Syndrome.
Who is at Risk for Patellofemoral Syndrome?
While athletes, particularly runners and jumpers, are most at risk, anyone can develop Patellofemoral Syndrome. It’s more common in individuals who engage in repetitive knee-bending activities or those who experience muscle imbalances or structural abnormalities.
Symptoms of Patellofemoral Syndrome
Identifying Patellofemoral Syndrome often starts with recognizing its characteristic symptoms. The most common signs include:
- Knee Pain: Pain at the front of the knee, especially during activities like running, squatting, or climbing stairs.
- Swelling: Mild swelling around the kneecap may be present in some cases.
- Grinding Sensation: A sensation of grinding or "popping" when moving the knee, especially after prolonged sitting or bending.
- Pain After Inactivity: Discomfort is often worse after periods of inactivity, like sitting for a long time, and can worsen with overuse.
Diagnosing Patellofemoral Syndrome
Diagnosis usually begins with a clinical evaluation. A healthcare professional will examine your knee's range of motion, alignment, and stability. They might also assess your gait and the strength of surrounding muscles to identify any imbalances or structural issues contributing to the condition.
In some cases, imaging tests like X-rays or MRIs may be used to rule out other causes of knee pain, such as ligament injuries or arthritis.
Non-Surgical Treatments for Patellofemoral Syndrome
The good news is that many people can manage Patellofemoral Syndrome with non-surgical treatments. Here are some of the most effective methods for treating this condition:
Physical Therapy
Physical therapy is the cornerstone of treatment for Patellofemoral Syndrome. A physical therapist can guide you through exercises that strengthen the muscles around the knee, improving alignment and reducing strain on the joint. Some common physical therapy goals include:
- Quadriceps Strengthening: Strengthening the quads can help better align the patella and reduce pressure on the knee joint.
- Hip Strengthening: Strengthening the muscles of the hip and glutes helps support the knee and improve overall biomechanics.
- Stretching: Stretching the hamstrings, calves, and iliotibial (IT) band can relieve tension and improve knee mobility.
R.I.C.E. Method
In the acute phase, the R.I.C.E. method (Rest, Ice, Compression, Elevation) can help reduce pain and inflammation. Resting the knee allows it to heal, while ice and compression reduce swelling.
Orthotics and Bracing
For those with structural abnormalities, custom orthotics can provide support and correct misalignments that contribute to PFS. Knee braces or taping techniques may also be used to stabilize the patella and reduce discomfort.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Over-the-counter NSAIDs, like ibuprofen or naproxen, can help manage pain and reduce inflammation, especially during the early stages of recovery.
Surgical Treatment for Patellofemoral Syndrome
In severe or persistent cases where non-surgical treatments fail, surgical intervention might be necessary. Surgery is usually recommended only after all other options have been exhausted.
Arthroscopy
In some cases, an arthroscopic procedure may be performed to remove damaged tissue, realign the kneecap, or repair soft tissue damage. This minimally invasive surgery involves small incisions and offers a quicker recovery time compared to traditional open surgery.
Realignment Surgery
In rare cases where the misalignment is severe, a more invasive procedure, such as a tibial tubercle transfer, may be required to reposition the patella and correct tracking issues.
Preventing Patellofemoral Syndrome
Preventing Patellofemoral Syndrome is all about maintaining strong, balanced muscles around the knee and addressing biomechanical issues early on.
1. Strengthening and Conditioning
Strengthen your quadriceps, hamstrings, and hip muscles to ensure proper knee alignment. Incorporating lower body strength training into your workout routine can help prevent muscle imbalances.
2. Proper Footwear and Orthotics
Wearing supportive shoes and using custom orthotics can correct biomechanical issues like flat feet or high arches, reducing the risk of developing PFS.
3. Warm-Up and Stretching
Always warm up before physical activity and incorporate regular stretching to maintain flexibility in the muscles surrounding the knee. This can prevent strain on the patella.
4. Modify High-Impact Activities
If you’re prone to knee pain, consider modifying high-impact activities. Instead of running on hard surfaces, try softer surfaces or switch to low-impact exercises like swimming or cycling to minimize stress on the knees.
Recovery and Rehabilitation
Recovery from Patellofemoral Syndrome varies depending on the severity of the condition and the treatment approach. With non-surgical treatments, most people start to notice improvement within a few weeks to a few months. The key is to stick with your physical therapy routine and make gradual adjustments to your activity levels.
If surgery is necessary, recovery may take longer, with most individuals returning to full activity within 4 to 6 months, depending on the procedure performed.
Conclusion: Is Patellofemoral Syndrome Affecting Your Life?
Patellofemoral Syndrome doesn’t have to keep you on the sidelines. With the right treatment plan—whether that’s physical therapy, orthotics, or surgery—you can alleviate your pain and get back to the activities you love. If you suspect you have PFS, consult with a specialist to explore your treatment options and begin your recovery journey.
Frequently Asked Questions
1. What causes Patellofemoral Syndrome?
Patellofemoral Syndrome is typically caused by overuse, muscle imbalances, or structural abnormalities that lead to improper tracking of the kneecap, causing pain and irritation.
2. How long does it take to recover from Patellofemoral Syndrome?
With proper treatment, recovery from Patellofemoral Syndrome can take anywhere from a few weeks to several months. Early intervention and consistent physical therapy can speed up recovery.
3. Can Patellofemoral Syndrome be cured without surgery?
Yes, most cases of Patellofemoral Syndrome can be treated with non-surgical methods like physical therapy, orthotics, and lifestyle modifications.
4. What exercises are good for Patellofemoral Syndrome?
Strengthening exercises for the quadriceps, hip, and glute muscles, along with stretching the hamstrings and IT band, are beneficial for managing PFS. A physical therapist can guide you through the right exercises.
5. When should I consider surgery for Patellofemoral Syndrome?
Surgery is generally considered when non-surgical treatments fail to provide relief, and the pain is significantly affecting your quality of life. A healthcare professional will help you determine if surgery is necessary.
Sources:


